Experience of Using Silicone Gel Sheet (Lady Care3) for Laparoscopic Surgical Wounds: An Investigation into Safety and Efficacy
Toshiyuki Kakinuma*, Kaoru Kakinuma, Yoshio Matsuda, Ikuo Sato, Kaoru Yanagida, Michitaka Ohwada
Department of Obstetrics and Gynecology, International University of Health and Welfare Hospital, Japan.
*Corresponding author: Toshiyuki Kakinuma, Department of Obstetrics and Gynecology, International University of Health and Welfare Hospital, 537-3 Iguchi, Nasushiobara, Tochigi 329-2763, Japan. Tel: +81-287-39-3060; Fax No.: +81-287-39-3001; Email: tokakinuma@gmail.com
Citation: Kakinuma T, Kakinuma K, Matsuda Y, Sato I, Yanagida K (2020) Experience of Using Silicone Gel Sheet (Lady Care3) for Laparoscopic Surgical Wounds: An Investigation into Safety and Efficacy. Annal Cas Rep Rev: ACRR-109.
Received Date: 03 April, 2020; Accepted Date: 09 April, 2020; Published Date: 17 April, 2020.
Abstract
Background and Objective: While there has been an increase in the number of laparoscopic surgery in Japan, few studies have reported about scars from wounds by laparoscopic surgery. Silicone gel sheets are widely used as part of multidisciplinary treatment for hypertrophic scars and keloids, and their usefulness has been reported. The present study examined the efficacy and safety of a silicone gel sheet (Lady Care3) for laparoscopic surgical wounds.
Subjects and methods: Subjects were 15 cases who underwent laparoscopic surgery during the period from March 2017 to March 2018. Silicone gel sheets (Lady Care3) were applied to the wounds (umbilicus, lower abdomen) for one week to six months postoperatively. The JSW Scar Scale was used in evaluating the wounds. The wounds were evaluated visually and through interviews before the application of silicone gel sheets, at three months following surgery, and six months following surgery.
Results: The JSW Scar Scale scores for the umbilicus surgical wound were 7.4±2.4 before application, 2.7±1.6 at three months following surgery, and 0.9±0.7 at six months following surgery. Those for the lower abdomen surgical wounds were 4.7±2.3, 0.8±1.1, and 0.3±0.5, respectively. Three cases reported pruritus; however, all were mild, and it was tolerable to continue to use silicone gel sheets in those cases.
Conclusion: Significant decreases were observed in the JSW Scar Scale scores from an early postoperative stage, and no serious adverse events were observed. Therefore, the present study suggested that the silicone gel sheet (Lady Care3) is safe and efficacious.
Keywords: Hypertrophic scar, keloid, silicone gel sheet, laparoscopic surgery
Introduction
When the skin suffers damage due to trauma or surgery, the wound healing mechanism, which includes processes such as inflammatory cell infiltration, angiogenesis, and regeneration of the extracellular matrix, is triggered. Hypertrophic scarring and keloids are types of fibroproliferative disease that present as redness caused by the overproduction of collagen fibers by fibroblasts during the wound healing process. These conditions are accompanied by itching and pain, as well as severe psychological stress placed on the patient by the cosmetic problems these conditions cause. Thus, their prevention is an important consideration. Silicone gel sheeting has come into widespread use as part of multidisciplinary treatment of hypertrophic scars and keloids, and studies have reported that they are effective in the prevention of these conditions after Cesarean section.
The number of laparoscopic surgeries performed in Japan in increasing annually, but few studies have investigated the issue of surgical wound scarring. Here, we report on the effectiveness and safety of silicone gel sheeting (Lady Care 3) when used on laparoscopic surgical wounds.
Subjects and Methods
This study was conducted after receiving the approval of this hospital’s Institutional Review Board ethical review number (13-B-384). The subjects were 15 patients who underwent laparoscopic surgery between March 2017 and March 2018. Laparoscopic surgery was performed by inserting a 5 mm trocar (ENDOPATH® Trocar System, Johnson & Johnson, Tokyo) for closed trocar entry into the umbilicus using the 4-port parallel method (Figure. 1).
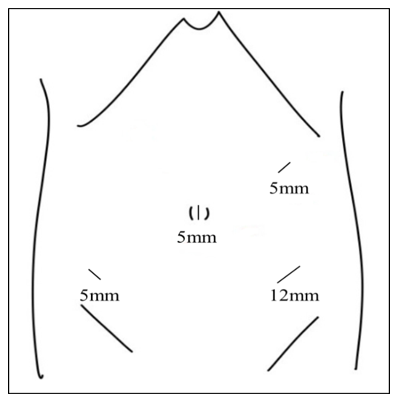
Figure 1: Trocar insertion sites.
After the laparoscopic surgery was completed the trocar was removed and a 12 mm trocar (for two layers of rectus abdominis muscle layer subcutaneous tissue) and a 5 mm trocar (for the subcutaneous tissue only) to suture the surgical wound (round body needles, 2-0 absorbable suture [VICRYL® Johnson & Johnson, Tokyo]). The epidermis was closed using dermatological adhesive tape (DERMABOND® Advanced, Johnson & Johnson, Tokyo). During a period between one week and six months after surgery, silicone gel sheeting (Lady Care 3, Gyne Mom Co., Ltd., Saitama; Fig. 2) was affixed to the surgical wounds (umbilicus, lower abdomen) of 15 patients in the Silicone group.

Figure 2: Lady Care 3 (Gyne Mom Co., Ltd.)
Surgical wound assessment was done in both groups at three time points (post-1W, post-3M, post-6M) using the JSW Scar Scale (Table 1). The scores were converted to numerals for the purpose of comparison. Statistical analyses were performed using the student’s t-test and the chi-squared test. Statistical significance was set at P<0.05.
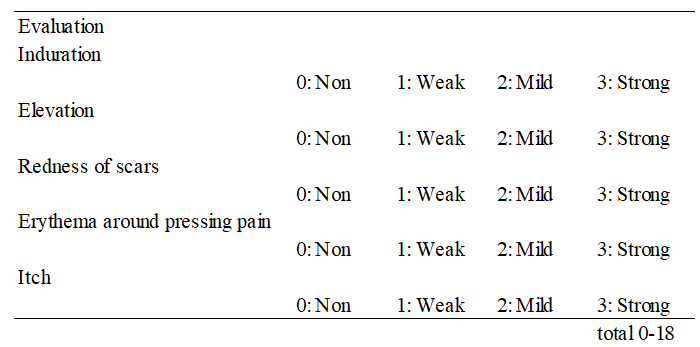
Table 1: JSW Scar Scale 2011 (Classification and Evaluation of Keloids and Hypertrophic Scars).
Results
Mean age was 45.7±13.1 years, Body mass index (BMI) was 23.0±4.1. The breakdown of laparoscopic surgery included 6 laparoscopic total hysterectomy, 1 laparoscopic myomectomy, 4 laparoscopic appendectomy, and 4 laparoscopic ovarian tumor resection. JSW Scar Scale scores for the umbilicus surgical wound were 7.4±2.4 (pre-affixation: post-1W), 2.7±1.6 (post-3M), and 0.9±0.7 (post-6M). JSW Scar Scale scores for the lower abdomen surgical wounds were 4.7±2.3, 0.8±1.1, and 0.3±0.5 respectively (Fig. 3).
The JSW Scar Scale scores for the post-3M time point (both umbilicus and lower abdomen wounds) were significantly lower than at pre-affixation (post-1W).
Although no serious adverse events occurred in the Silicone group, three patients experienced itchiness (Fig. 3).
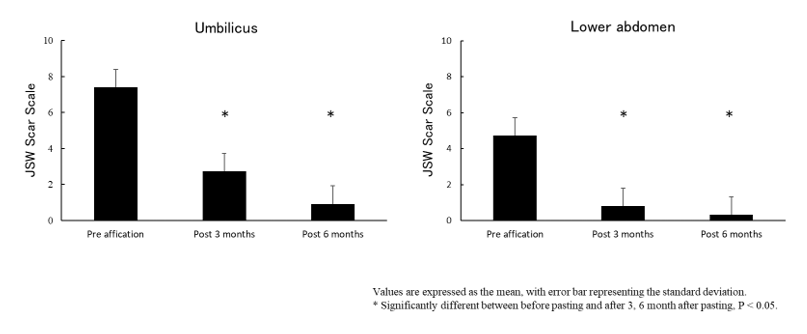
Figure 3: Variations in JSW Scar Scale scores.
Discussion
Hypertrophic scarring and keloids are frequently observed in daily medical practice. Hypertrophic scarring in particular commonly occurs at surgical wound sites, and as a result they are a problem likely to be faced by all surgical specialists. In addition to associated itching and pain, patients often suffer a great deal of psychological stress due to cosmetic problems associated with such scarring, and therefore it is often advisable to have “scar-less healing” as a goal.
When the skin is damaged as a result of trauma or surgery, the wound healing mechanism, which includes processes such as inflammatory cell infiltration, angiogenesis, and regeneration of the extracellular matrix, is triggered. Normally, the redness that occurs at the wound site gradually disappears, and then is replaced by a white-colored mature scar. In cases of hypertrophic scarring and keloids, some instigating factor during the course of the wound healing process causes wound healing to be delayed and the wound to be maintained over a longer than normal period of time. Possible instigating factors include foreign objects, infections, mechanical irritation, genetic factors, wound-delaying factors, cytokines, and hormones [1-5]. However, the specific causes remain unknown.
Several treatments are available for hypertrophic scarring and keloids, including pharmacotherapy, compression therapy, surgery, cryotherapy, radiotherapy, and laser therapy, and in many cases multiple therapies are utilized. However, these conditions are often difficult to treat and manage, and thus effort must be made to prevent their occurrence.
Since silicone gel sheet therapy was first reported as a novel treatment of post-burn scarring in children by Perkins et al. in 1982 [6], it has come into clinical use in the treatment of hypertrophic scarring and keloids. Although its mechanism of action remains unknown, much discussion of this has taken place over the years. Quinn reported that the speed at which water vapor moved at the sites where silicone gel sheeting had been affixed was relatively slower than at the sites of scarring [7]. Katz and Davey et al. reported that acts as an alternate stratum corneum, which they assumed reduced the loss of water vapor and reduced collagen proliferation and capillary activity [8-9]. Suetake et al. compared the stratum corneum functioning at sites where silicone gel sheeting was affixed and sites where plastic film (vinylidene chloride) was affixed, and they reported that the fact that the film sites contained more moisture in the stratum corneum suggests that the silicone gel sheeting ensures a level of moisturization that is conducive to improvement in symptoms [10].
On the other hand, in addition to the moisturizing effect, it is also conceivable that direct external force applied to the scar site by the silicone gel sheeting may have a protective effect, or that the protective effect may arise from the excessive traction placed on the surrounding tissue and this external stimulation also may explain the protective effect of silicone gel sheeting.10) In addition, many types of plastic film utilize organic solvents as adhesives and as a result when they are used on hypertrophic scars or keloids problems such as peeling away of the stratum corneum and contact dermatitis may occur. However, silicone gel sheeting is less likely to cause these problems, and thus it is conceivable that silicone gel may allow the epidermis to rest. Physical protection from direct external irritation from clothing and preventing the patient from scratching the scar site may also alleviate symptoms.
Currently, none of the various theories that have been presented as explanations for the mechanism of action of silicone gel sheeting on hypertrophic scars and keloids have been completely verified and none have been shown to have specificity with regard to these conditions. However, according to a number of reports, the moisturizing effect that protects the epidermis from dryness, the physical protection of the surface of the skin they provide, the physical protective effect they have that allows the tissues underneath to rest, and the mechanical effect of placing traction on the surrounding tissues which allows the scar site to rest are all conceivable explanations as they all are related to protection of the scar site and to allowing the site to rest.
Data have suggested that silicone gel sheets, which are a therapeutic material that is widely used as part of the multidisciplinary treatment of hypertrophic scarring and keloids, are effective in the prevention of postoperative development of hypertrophic scarring and keloids [11] In their study of prevention of the development of fibrous hypertrophic scarring and keloids, Gold et al. reported Chan et al. reported that in the silicone gel usage group itching, pain, scar height, redness, and hardness all showed that there was a significant protective effect on the scar tissue [12]. In the present study of the efficacy of silicone gel sheeting on laparoscopic surgical wounds, we also found that at post-3M the JSW Scar Scale scores in the Silicone group were significantly lower, indicating that the wounds had improved faster than in the Control group.
The Lady Care 3 that we utilized in the present study is a soft skin adhesive silicone gel sheet for medical use whose main components have been registered with the Drug Master File (DMF) of the US Food and Drug Administration (FDA), as is the case with the entire Lady Care series product line. It was developed for use after laparoscopic surgery and is elliptical in shape and measures 30 mm in diameter. The previous products in the Lady Care series have already been used in the prevention of the formation of hypertrophic scarring after Cesarean section. As is the case with the other products in the Lady Care series, Lady Care 3 is pliable and can be affixed in a way that allows it to be formed to the shape of the body where it is being used, which in turn allows it to directly adhere to the affected site. As it is durable, it can be removed prior to bathing and replaced, which means that it is reusable. Normally, a single sheet can be used for 1-2 months. Problems associated with its use include the fact that during seasons when people experience increased sweating, such as the summer, the adhesiveness of the silicone gel sheeting can be reduced or lost, and itching has been reported by many patients. In the present study we found that itching occurred during use of the Lady Care 3 sheets in three patients (20%). All cases were mild and continued use of the product was possible. However, we believe it is necessary to devise a thinner silicone gel sheet that allows sweat to be wiped off more frequently. Currently, a thinner version of the Lady Care 3 sheet that has stronger adhesiveness is under development, and thus we hope to study this new product in the future with larger numbers of study subjects and over a longer observation period.
Conclusion
The fact that the JSW Scar Scale score in the Silicone group was significantly lower sooner after surgery than the Control group, and the fact that there were no serious adverse events associated with the use of the silicone gel sheet, suggest that the silicone gel sheeting (Lady Care 3) is both safe and effective.
There is no conflict of interest in this study.
Reference
- Ogawa R, Okai K, Tokumura F, Mori K, Ohmori Y, et al. (2012) The relationship between skin stretching/contraction and pathologic scarring: the important role of mechanical forces in keloid generation. Wound Repair Regen 20:149-57.
- Moles A, Hamel O, Perret C, Bord E, Roger Robert R, et al. (2014) Symptomatic vertebral hemangiomas during pregnancy. J Neurosurg Spine 20: 585-591.
- Quong WL, Kozai Y, Ogawa R (2017) A Case of Keloids Complicated by Castleman’s Disease: Interleukin-6 as a Keloid Risk Factor. Plast Reconstr Surg Glob Open 5: e1336.
- Nakashima M, Chung S, Takahashi A, Kamatani N, Kawaguchi T, et al. (2010) A genome-wide association study identifies four susceptibility loci for keloid in the Japanese population. Nat Genet 42: 768-771.
- Ogawa R, Watanabe A, Than Naing B, Sasaki M, Atsushi Fujita A, et al. (2014) Associations between keloid severity and single-nucleotide polymorphisms: importance of rs8032158 as a biomarker of keloid severity. J Invest Dermatol 134: 2041-2043.
- Perkins K, Davey RB, Wallis KA (1983) Silicone gel: a new treatment for burn scars and contractures. Burns Incl Therm Inj 9: 201-204.
- Quinn KJ (1987) Silicone gel in scar treatment. Burns Incl Therm Inj 13: 33-40.
- Katz BE (1995) Silicone gel sheeting in scar therapy. Cutis 56: 65-67.
- Davey RB, Wallis KA, Bowering K (1991) Adhesive contact media–an update on graft fixation and burn scar management. Burns 17: 313-319.
- Suetak T, Sasai S, Zhen YX, Tagami H (2000) Effects of silicone gel sheet on the stratum corneum hydration. Br J Plast Surg 53: 503-507.
